Home » Blog
Category Archives: Blog
Breastfeeding for Dads and Grandmas
This is a blog which I wrote for the new Human milk page Tailor made for Tiny Humans http://human-milk.com/
Wendy Jones Blog – Breastfeeding for Dads and Grandmas
I’ve just spent the Christmas holidays with my daughters, their partners and 3 grandchildren, two of whom are still being breastfed (21 months and 6 months). Having just had a new book published called Breastfeeding for Dads and Grandmas it made me think how different our holidays were in a very pro breastfeeding family than they might be in other families?
The son in law who has yet to have children, is totally comfortable with sitting next to his sisters in law as they breastfeed and has been immeasurably supportive to his own sister. She was going to “give breastfeeding a go” but is now as committed as our family and doesn’t understand why anyone would feed in any other way.
However, the number of emails and Facebook messages from mothers suffering from anxiety since Christmas has reached unbelievable levels – on average 3 a day every day. Why might that be I wondered?
I suspect that for many other mothers spending longer than usual in close proximity to the extended family can be stressful. The emotions seem to run at fever pitch in the Festive Season – everyone wants it to be perfect. Most of us spend too much, eat too much, drink too much, don’t exercise as much and generally suffer from “liverishness” as my Grandma used to term it (usually with an added “everyone could do with a good dose of syrup of figs!”).
Nevertheless in this hot pot of emotion, parents try to manage their babies needs for quiet to feed or sleep, not to be cuddled by Great Aunt Ethel when they want Mum, don’t want to eat the rich offerings of solids suitable for babies (really?).
Inevitably the subject of infant feeding gets raised at some point during the visit. In our very pro-breastfeeding house the mums were supported. But what if you are with mother-in-law who formula fed your partner and makes no secret of her distaste of breastfeeding? How does your partner feel? How do you feel/ Desperate to keep the peace he might seem to agree with his mother. Neither of you wants to get into an argument but you are both secure in your decision to breastfeed. It is difficult isn’t it? If the baby cries you hear the comment “is he hungry again? Your milk can’t be good enough”. You are feeding quietly “what again? Surely you can’t have enough milk”. Feeding late at night/overnight/co-sleeping “When my children were babies they were in bed by 6pm and we didn’t hear from them again till 8am”. And Heaven forfend that you should dare to continue breastfeeding into toddlerhood!
It is no surprise that come January these new mums are anxious and more than a little depressed. Being a mum isn’t easy, these babies don’t read the books and don’t abide by any rules. Each baby is an individual and will reach his/her milestones in their own sweet time. Cherish every milky moment, every snuggle, every smile as all too soon they will grow up. When you feel that someone is criticising you smile sweetly, acknowledge the comment but then LET IT GO. This is your baby, you make the decisions. The advice on timing of feeds, weaning, sleeping has all changed dramatically in the fast 35 years (I know because I have been a mum in this time and gone on to support lots of others). It’s ok to breastfeed for comfort as well as nutrition, there is no such thing as using the nipple as a dummy, it is ok to co sleep if you want, it’s equally ok not to if you choose, it is also ok to ignore the advice of your mother, mother in law or Great Aunt Ethel!
Oh, cleaning and scrubbing will wait till tomorrow,
But children grow up, as I’ve learned to my sorrow.
So quiet down, cobwebs. Dust, go to sleep.
I’m rocking my baby. Babies don’t keep.
Song for a Fifth Child (Babies Don’t Keep)
by Ruth Hulburt Hamilton

Breastfeeding and Chronic Medical Conditions
Today is my birthday but I decided I wanted to share my day with the wider world so I have decreased the price of Breastfeeding and Chronic Medical Conditions. The paperpack is now £9.99 instead of £14.99 and the kindle reduced to £4.99 from £9.99 . I hope that it answers many of the questions asked including painkillers, antibiotics and procedures as well as breastfeeding problems and the many medical conditions.

Anxiety and Covid-19 (Coronavirus)
Currently we are all anxious – Covid-19 is changing everything so rapidly and life is uncertain in so many aspects. On the drugs in breastmilk service we are receiving lots of queries about natural remedies for anxiety – Bach flower remedy, Kalms etc – and lots of supplements believed to have powers to protect. These queries are hard to deal with. Sometimes we have anecdotal information but rarely evidence that these are compatible with breastfeeding. It is hard for us to say we don’t know but we hope you understand why we can’t help.
Other ways to deal with anxiety
- Anxiety UK launched a You Tube on living with uncertainty – shorturl.at/qEIL8
- Headspace has a module on anxiety which may help you ground yourself by listening to your breathing.
- There are online CBT modules listed https://www.breastfeedingnetwork.org.uk/anxiety/ and much sensible information.
- Talk to others and share your anxiety but don’t dwell on it. Most people will develop only mild symptoms.
If I had one thing to share it would be – stay off social media which will probably fuel your anxiety. Listen to the news but not too often. We are in this situation for the long haul sadly and anxiety is exhausting. Enjoy every moment with your baby, value the oxytocin, watch your baby and not your phone. Sadly, there is no magic wand to relieve the anxiety and what-ifs just now. Life is changing daily.
- Do wash your hands with soap and water often –for at least 20 seconds
- Always wash your hands when you get home or into work or after going outside the house
- Use hand sanitiser gel if soap and water are not available
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when you cough or sneeze or sneeze into your elbow (but change clothes as soon as possible).
- Dispose of used tissues in the bin immediately and wash your hands afterwards
- Avoid close contact with people who are unwell
- If you or a member of your family develop a fever or sudden onset cough self-isolate for 14 days and take paracetamol (ibuprofen currently not recommended although evidence of risk is low self help treatment coronovirus)
Don’t touch your eyes, nose or mouth if your hands are not clean. There is no need to stop breastfeeding UNICEF and Covid 19, ABM statement on coronovirus 2019,
Keep an eye on the Public Health England information which us updated regularly.
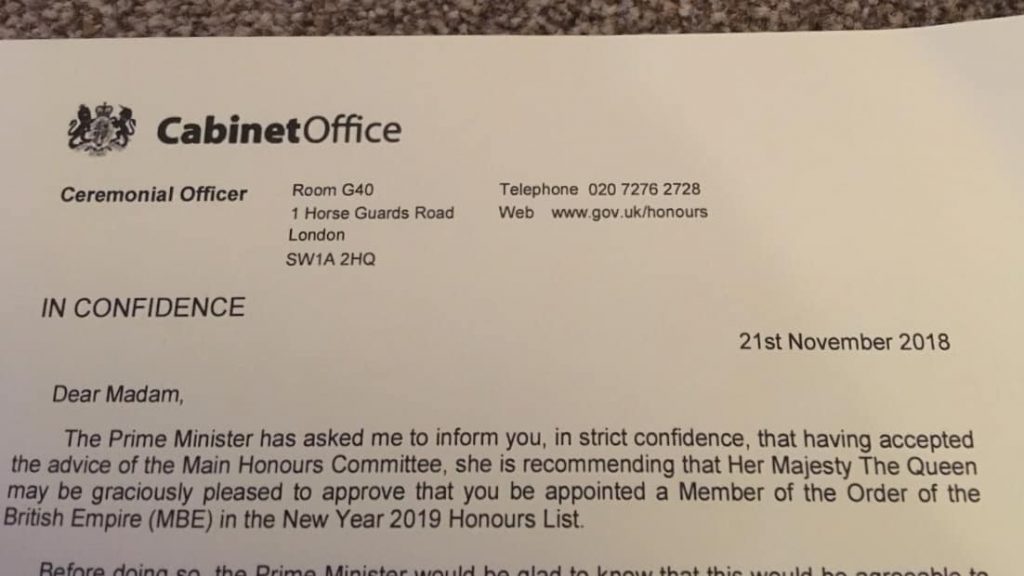
Wendy Jones MBE
That new title is going to take a lot of getting used to! I am very proud and delighted to have been nominated for an MBE for services to mothers and babies as a founder of the Breastfeeding Network Drugs in Breastmilk Service. I never thought this would happen to me following a path which I didnt really plan 22 years ago but has led me to this amazing place. I feel inspired to keep going and hopefully change some more professional attitudes that prescribing a medication doesnt mean that a mother needs to interrupt breastfeeding. Thank you to the many, many people who have sent messages of congratulations today – I appreciate them so much.
I also want to thank my wonderful family for their support – my husband Mike, my daughters Kerensa, Bethany and Tara, my son in laws Christian, Steve, Rich and Ian and of course my treasured grandchildren Stirling, Isaac, Beatrix and Elodie and the new bump due in 2019. I cant tell you how much I love you all
Change the conversation about medicines and breastfeeding
I spend on average 4 full hours across every day providing info to mums told they HAVE to stop breastfeeding to take medicines. Do more people know about the drugs in breastmilk service or are professionals less willing to take risks so stopping breastfeeding seen as best option? How can we change the conversation ?
Where does it make sense to tell mothers stop breastfeeding to take medicines when we have specialist support texts and services? Breastfeeding has HUGE advantages for mums, babies and the economy. We need to listen, support and provide evidence based info for all mums breastfeeding and formula feeding not rely on manufacturers
There are economic savings for the health economy. Renfrew (2012) provided a detailed cost analysis of potential savings, reductions in hospital admissions and GP appointments:
Assuming a moderate increase in breastfeeding rates, if 45% of women exclusively breastfed for four months, and if 75% of babies in neonatal units were breastfed at discharge, every year there could be an estimated:
- 3,285 fewer gastrointestinal infection-related hospital admissions and 10,637 fewer GP consultations, with over £3.6 million saved in treatment costs annually
- 5,916 fewer lower respiratory tract infection related hospital admissions and 22,248 fewer GP consultations, with around £6.7 million saved in treatment costs annually
- 21,045 fewer acute otitis media (AOM) related GP consultations, with over £750,000 saved in treatment costs annually
- 361 fewer cases of NEC, with over £6 million saved in treatment costs annually.
In total, over £17 million could be gained annually by avoiding the costs of treating four acute diseases in infants. Increasing breastfeeding prevalence further would result in even greater cost savings”
In addition, if half those mothers who currently do not breastfeed were to breastfeed for up to 18 months in their lifetime, for each annual cohort of around 313,000 first-time mothers there could be:
- 865 fewer breast cancer cases with cost savings to the health service of over £21 million, 512 breast cancer-related quality adjusted life years (QALYs) would be gained, equating to a value of over £10 million.
This could result in an incremental benefit of more than £31 million, over the lifetime of each annual cohort of first-time mothers.
Raynaud’s and Breastfeeding
Raynaud’s phenomenon affects up to 10% of otherwise healthy women aged 21-50 years of age. It is 9 times more common in women than men.
Yet many doctors are unaware that Raynaud’s can affect breastfeeding. It produces deep pain after feeds with a mother often automatically covering her nipples or massaging them to restore the blood flow. Symptoms are often mis-diagnosed as thrush when in fact the use of fluconazole can make the symptoms worse by causing further vasoconstriction.
Most mothers who experience problems with Raynaud’s during breastfeeding, have a history of cold hands and feet or a close relative who has. It may be that in a family it is routine to wear thick socks and gloves, maybe a vest without realising that they may be “unusual” in their response to the cold.
Babies of mothers with Raynaud’s may be born early and / or smaller because of restriction of blood flow to the placenta. It is not uncommon for there to be a maternal (or close family) history of migraines.
Symptoms which differentiate Raynaud’s phenomenon with other causes of breast pain are:
- Pain in both breasts after feeds
- Pain which may be precipitated by being cold or for example going down the freezer aisle in a supermarket
- Rapid 3 colour change in the nipples after feeds

- Pain that is resolved by warmth or gentle massage
- A history or close family history of poor circulation
Treatment of Raynaud’s during breastfeeding
- Don’t ignore the fact that pain after breastfeeds may be due to less than perfect attachment of the baby at the breast. A white tip to the nipple after feeds is not the same as the tri colour change typical of Raynaud’s
- Nifedipine 30mg a day (either as 10mg three times a day or long acting 30mg once daily. The amount in breastmilk is too small to affect babies although it may give the mother hot flushes and / or headaches. The following extract is taken from Breastfeeding and Medication 2nd Ed to be published May 2018
- High doses of vitamin B6 (Newman 2012), magnesium (Smith 1960, Turlapaty Leppert1994), calcium (DiGiacomo 1989), fatty acids (Belch 1985) and fish oil supplementation (DiGiacomo 1989) have also been suggested but take a minimum of 6 weeks to be effective. Ginger 2000mg-4000mg daily. Capsules usually contain 500mg. It may also be beneficial to add ginger to your diet, to drink ginger tea, or to put a spoonful of ground ginger in your bathing water (Royal Free hospital www.royalfree.nhs.uk/pip_admin/docs/Raynaudsnatural_186.pdf)
Nifedipine
Nifedipine relaxes vascular smooth muscle and dilates coronary and peripheral arteries. It has activity in reducing blood pressure and in the treatment of Reynaud’s syndrome
Nifedipine is almost completely absorbed from the GI tract but undergoes extensive first-pass metabolism. It is up to 98% bound to plasma proteins. It is used to treat hypertension (Penny and Lewis 1989; Ehrenkranz et al. 1989) and also to improve circulation in Reynaud’s disease (cold extremities and nipple vasospasm) in doses up to 30 mg daily (Lawlor-Smith and Lawlor-Smith 1996; Garrison 2002; Anderson et al. 2004). Side effects for the mother include flushing and headache, which may limit its usefulness. It is present in breastmilk but in levels too small to be harmful and there have been no reports of adverse effects in babies (see Chapter 5).
In Taddio et al’s study (1996) of 21 women taking 40 mg daily the babies were estimated to be exposed to 0.1% of the maternal weight adjusted dose via breastmilk. Nifedipine is widely used to treat pre-eclampsia and eclampsia in the mother together with methyldopa or a beta blocker. Ehrenkranz et al. (1989) studied one woman who took 10, 20 or 30 mg three times daily on different days. Using the maximum dose transferred by the 30 mg regimen, the authors estimated that the baby would be exposed to the authors estimated that an exclusively breastfed infant would receive an estimated maximum of 7.5 µg per kilogramme of nifedipine daily. Its relative infant dose is quoted as 2.3–3.4% (Hale 2017 online access).
The BNF reports that the amount secreted into breastmilk is too small to be harmful but that manufacturer advises it should be avoided.
Compatible with breastfeeding.
References
- Anderson JE, Held N, Wright K, Raynaud’s phenomenon of the nipple: a treatable cause of painful breastfeeding, Pediatrics, 2004;113(4):e360–4.
- Ehrenkranz RA, Ackerman BA, Hulse JD, Nifedipine transfer into human milk, J Pediatr, 1989;114:478–80.
- Garrison CP, Nipple vasospasm, Raynaud’s syndrome, and nifedipine, J Hum Lact, 2002;18(4):382–5.
- Lawlor-Smith LS, Lawlor-Smith CL, Raynaud’s phenomenon of the nipple: a preventable cause of breastfeeding failure?, Med J Aust, 1996;166:448. Letter.
- Penny WJ, Lewis MJ, Nifedipine is excreted in human milk, Eur J Clin Pharmacol, 1989;36:427–8.
- Taddio A; Oskamp M; Ito S; Bryan H; Farine D; Ryan D; Koren G,. Is nifedipine use during labour and breastfeeding safe for the neonate?, Clin Invest Med, 1996;19(4 Suppl.):S11. Abstract.

Public Health England Study and Medication during Breastfeeding
71% of 500 women who responded to a PHE study, think breastfeeding will limit the medication which can be taken! So lots of work for me still to do then. Could professionals buy a copy of Breastfeeding and Medication to reassure women?
Statements like this on the NHS site arent going to help – more about manufacturer protecting themselves? Not taking risks? Could be better worded as it just isnt true. Breastfeeding mothers with depression get treated every day and their babies are fine!
“Breastfeeding: As a precaution, the use of antidepressants if you’re breastfeeding isn’t usually recommended. However, there are circumstances when both the benefits of treatment for depression (or other mental health conditions) and the benefits of breastfeeding your baby outweigh the potential risks. If you’re treated with antidepressants when breastfeeding, then paroxetine or sertraline is normally recommended.”
The Start for life page https://www.nhs.uk/start4life/breastfeedingto which the chat box https://www.messenger.com/t/Start4LifeBreastFeedingFriend/ links identifies the BfN Drugs in breastmilk helpine which I run as a resource. But they dont fund it – it is run on a voluntary basis and they didnt ask permission to see if I can deal with additional work. But I will keep doing my best to support mothers who need medication whilst breastfeeding
” Almost three-quarters of women in England start breastfeeding after giving birth but less than half are still doing so two months later, according to NHS and Public Health England data.
PHE recommends exclusive breastfeeding for the first six months, as does the World Health Organisation, because it boosts a baby’s ability to fight illness and infection. But a comparison of initial breastfeeding rates and those after six to eight weeks in the final quarter of 2015 found that they were 40% lower for the latter (44% compared with 73%).
A survey of 500 mothers commissioned by PHE found that fears about breastfeeding among women included that it could be painful (74%), prevent them taking medication (71%) and be embarrassing in front of strangers (63%).
The PHE’s chief nurse, Viv Bennett, said: “We can all help women feel comfortable breastfeeding their baby wherever they are. Creating a wider culture of encouragement and support will help make a mother’s experience all the more positive.”
PHE has launched an interactive breastfeeding friend chatbot, accessed through Facebook messenger, to provide personal support for breastfeeding 24 hours a day. Bennett said it would help women through the “crucial” initial period, after which things generally became easier.
A study published in the Lancet last year found the UK had the lowest rate of breastfeeding in the world, with only one in 200 women breastfeeding their children after they reach their first birthday.
The WHO recommends that breastfeeding form part of a baby’s diet up to two years of age. As well as reducing the likelihood of babies getting diarrhoea and respiratory infections, breastfeeding also lowers a mother’s risk of ovarian and breast cancer and burns about 500 calories a day.
The results, published on Thursday, suggested high-profile figures who promote breastfeeding can have a positive influence on other mothers. Just under half of respondents said the example of household names such as The Only Way is Essex star Sam Faiers, broadcaster Fearne Cotton and actor Blake Lively, who have recently championed breastfeeding on social media, had inspired them to do so themselves. About two-thirds (64%) said they felt more confident to breastfeed in public because of celebrity mums.
Other concerns raised by more than half of women were not being able to tell if their baby was getting enough or too much milk and that it could potentially place restrictions on the mother.
Jacque Gerrard, the director for England at the Royal College of Midwives, said: “Any initiative that goes towards helping mothers start and sustain breastfeeding for longer is positive as we know the health benefits from being breastfed last a lifetime.”
Breastfeeding and Medication
If you see breastfeeding mothers who need medication maybe you need to buy this book
https://www.amazon.co.uk/Breastfeeding-Medication-Wendy-Jones/dp/0415641063/ref=sr_1_1?ie=UTF8&qid=1489435817&sr=8-1&keywords=breastfeeding+and+medication
Training for Pharmacists
harmacists can access evidence based training for free rather than read material which is non evidence based and developed by the formula industry
https://www.academia.edu/26421451/The_pharmaceutical_care_of_breastfeeding_mothers?auto=download
Pharmacists can be as guilty as doctors in being influenced by the companies and inadvertently pass on negative messages about breastfeeding as described in this article Education and training of healthcare staff in the knowledge, attitudes and skills needed to work effectively with breastfeeding women: a systematic review
There are days when I despair at the information provided by my fellow professionals about infant feeding. Come on guys do some CPD on supporting breastfeeding mothers – it is a health issue and can save the NHS millions of pounds a year let alone morbidity and mortality of mothers and children.
Breastfeeding is a natural ‘safety net’ against the worst effects of poverty … Exclusive breastfeeding goes a long way toward cancelling out the health difference between being born into poverty and being born into affluence … It is almost as if breastfeeding takes the infant out of poverty for those first few months in order to give the child a fairer start in life and compensate for the injustice of the world into which it was born.
JAMES P. GRANT, EXECUTIVE DIRECTOR OF UNICEF (1980-1995)
https://www.unicef.org.uk/wp-content/uploads/sites/2/2012/11/Preventing_disease_saving_resources.pdf





